You should always have your own official book for your class whether it is from the Red Cross, ASHI or American Heart Association. The cool crew at CPR Florida also provides your free aha guidelines information, study guides and free videos for all CPR, First Aid, BLS, AED, Oxygen, Stop the Bleed, Narcane, Pet CPR, PALS and ACLS. We want to make you a hero in training!


NOTE: Those untrained in CPR can simply do chest compressions until help arrives.
1. Call: Check the victim for unresponsiveness. If there is no response, Call 911 and return to the victim. In most locations the emergency dispatcher can assist you with CPR instructions.
2. Pump: If the victim is still not breathing normally, coughing or moving, begin chest compressions. Push down on the chest 2 to 2.4 inches 30 times right between the nipples. Pump at the rate of 100-120/minute, faster than once per second (Continue or Repeat).
3. Blow: Tilt the head back and listen for breathing. If not breathing normally, pinch nose and cover the mouth with yours and blow until you see the chest rise. Give 2 breaths. Each breath should take 1 second.
Here is a full cpr scenario where the person actually is alive and talking to lifeguards stating he might have a heart attack...and he does within a few minutes. Watch real cpr video here now
Putting it all together. Here is complete adult cpr, aed, bag valve sequence. Complete cpr aed bvm bls sequence
The pulse check is no longer taught or expected of laypersons. Instead, if there is no response after two mouth-to-mouth breaths, begin to pump on the chest. Please note that the pulse check is still expected of health care providers. Remember, CPR is for those who have NO pulse and are NOT breathing. When you give CPR, you are giving them breaths and compressions. You give breaths to help give oxygen to the victim and you give chest compressions to act like their heart and help circulate the blood to the body.
If the victim DOES have a pulse, but they are not breathing, you do rescue breathing. Rescue breathing is giving breaths only. Give one breath every 5 seconds. This is for healthcare professionals only.
Check your child's breathing and pulse. Gently place him/her on their back on a firm surface. Make sure the airway is open by lifting the chin gently, then tipping the head back slowly. For 5-10 seconds, look, listen, and feel for signs of breathing. If they are not breathing, give two breaths and then do 30 compressions. (Healthcare professionals: To check for a pulse, gently place your first two fingers on the child's neck and feel for the carotid artery that's next to their throat. Feel for a pulse for 5-10 seconds. If there is a pulse, give one breath or use a bag-valve mask BVM every 3 seconds.)
If your child is not breathing and has no pulse, begin CPR: With your toddler still lying on their back, put the heel of your hand on the lower third of their breastbone (Use only 1 hand or use 2 hands, but do not press as hard or as deep as adult CPR). Depress the chest 1 1/2 inches (or 1/3 depth of the chest). Repeat 30 times within about 20 seconds (Count "one and two and three."). With your child's head still tilted, pinch their nose shut, put your mouth over their mouth, and give two slow, gentle breaths. Repeat the cycle of 30 compressions and 2 breaths. Click to see a quick Video of Child CPR
1. Shout and Tap : Shout and gently tap the child on the shoulder. If there is no response, position the infant on his or her back. Call 911
2. Compress then Breaths : Use 2-3 fingers in the center of the chest between the nipples to give 30 chest compressions going about 1.5 inches deep (or 1/3 depth of chest). If the baby is NOT breathing give 2 small gentle breaths. Cover the baby's mouth and nose with your mouth. Each breath should be about 1 second long. You should see the baby's chest rise with each breath. Continue 30 compressions and 2 puffs (breaths) and until EMS (911) arrives.
Healthcare Professionals: Check for a pulse in the inside of their arm (brachial pulse). If no pulse, do cycles of 30 compressions (using 2-3 fingers in the center of their chest between the nipples) and 2 breaths. Press down about 1.5 inches (or 1/3 the depth of the chest). Continue CPR until EMS arrives. If there is a pulse, give one breath every 3 seconds.
Click to see a Video of Infant CPR
Remove the object with your finger ONLY if you can see it! If your baby can't clear the airway on their own and you believe something is trapped there, carefully position the baby face down on your forearm, with your hand supporting the head and neck, and rest the arm holding the baby on your thigh. Support the baby so that the head is lower than the rest of their body. Then give five back blows between the shoulder blades with the heel of your hand to try to dislodge the object.
Next, place your free hand (the one that had been delivering the back blows) on the back of the head and along the spine and carefully turn the baby over supporting the head and neck. Support the baby face-up, with your forearm resting on your thigh, keeping the head lower than the rest of the baby's body. Place two or four fingers in the center of your baby's breastbone and give five chest thrusts, each about 1 inch deep. Continue the series of back blows and chest thrusts until the object is forced out, she begins to breathe on her own, she becomes unconscious, or advanced medical help arrives and takes over.
One person does bag valve mask and the other does the two hands encircling the chest technique to give 15 compressions and then 2 breaths. Remember, one person CPR for an infant is 2 breaths and 30 compressions. When two people are doing CPR, it is 2 breaths and 15 compressions.
How to help clear an obstructed airway in a conscious adult or child:
1. Determine if the person can speak or cough ( If not, proceed to the next step)
2. Just do abdominal thrusts or the Heimlich maneuver until the object comes out or the person passes out.
3. A chest thrust may be used for markedly obese persons or in late stages of pregnancy.
4. If the adult or child becomes unresponsive perform CPR if you see an object in the throat or mouth, remove it by doing a finger sweep.
5. Do CPR with finger sweep
If a child is choking, bend over and do the Heimlich. You can also go on both of your knees and perform the maneuver. Place one fist just above the child's navel with the thumb side facing the abdomen. Click for Photo Reference
View a Video of adult and child heimlich maneuver choking here
An AED is a device about the size of a laptop computer that analyzes the heart's rhythm for any abnormalities and, if necessary, directs the rescuer to deliver an electrical shock to the victim. This shock, called defibrillation, may help the heart to reestablish an effective rhythm of its own.
An AED is easy to operate. It uses voice prompts to instruct the rescuer. Once the machine is turned on, the rescuer will be prompted to apply two electrodes provided with the AED to the victim's chest. Once applied, the AED will begin to monitor the victim's heart rhythm. If a "shockable" rhythm is detected, the machine will charge itself and instruct the rescuer to stand clear of the victim and to press the shock button. The time to the first defibrillation shock is the most critical factor in determining survival rates for sudden cardiac arrest (SCA). With every minute that goes by, survival rates decrease by about 10%. That leaves a window of ten minutes in which to potentially save your life or the life of someone you know, after which survival rates average less than 2%. The best results for defibrillation occur in the first three minutes, measured from the moment the victim collapses to when the defibrillation shock is delivered. Click for Photo Reference
Put one pad on upper right of the chest and one on the lower left side of the body (side of body near stomach). When you place pads and then connect the cord, it will check for a shockable pulse. If there is a shockable pulse, it will say Shock Advised! If so, tell everyone to Clear! and then press shock. If no pulse, you press shock again. After 1 shock with no pulse, you MUST do CPR for 2 minutes and then let it reanalyze for a heart rhythm. Continue until EMS arrives.
Click for Video Demonstration of AED
Always start first aid with: Check, Call, Care.
"Check" the scene and see if anyone can help, to see if there is other dangers and safe for you to help them. "Call" 911 right away. Then give "Care" to the victim. Assess ABC's. Check their Airway, Breathing and Circulation:
1. Place the victim in shock position
2. Keep the person warm and comfortable
3. Turn the victim's head to one side if neck injury is not suspected
Shock is a life-threatening condition. Immediate medical care can make the difference between life and death.
Early signs of shock (most of which will be present) include:
1. Lightheadedness or a feeling that you are about to pass out
2. Restlessness, confusion, or signs of fear
3. Shallow, rapid breathing
4. Moist, cool skin or possibly profuse sweating
5. Weakness
6. Thirst, nausea, or vomiting
Also, a person in shock usually has an abnormal increase in heart rate and an abnormal decrease in blood pressure.
Late signs of shock include:
1. Changes in the person's level of consciousness, such as sudden unresponsiveness, faintness, loss of consciousness, or behavior changes.
2. A pale face or blue lips or earlobes.
Shock may occur in response to a sudden illness or injury. When the body loses too much blood or fluids, the circulatory system cannot get enough blood to the vital organs, and shock results. Shock is often associated with heavy external or internal bleeding from a serious injury. Spinal injuries can also cause shock. To help them, raise their feet 12 inches in the air and keep them calm and comfortable.
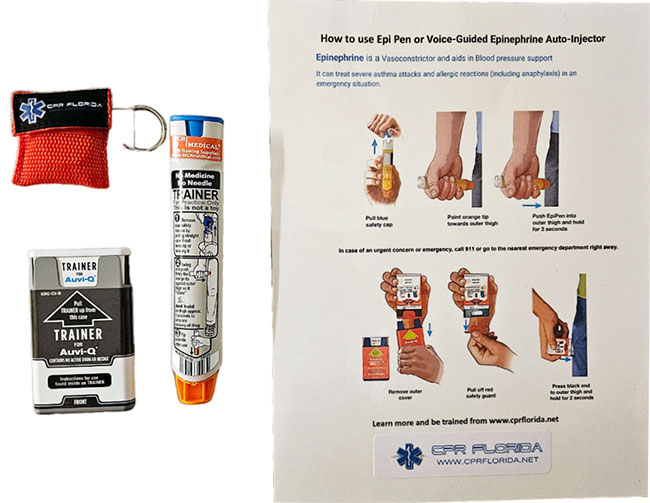
Many people have food allergies or are allergic to bites and stings. They may need an Epi Pen as soon as possible. An epi-pen has medicine inside a tube that has a needle. You place your hand around the pen (do not touch the bottom or top when using it), take off the top gray cap (round) and point the narrower end with the needle inside towards the person's leg. They can do it themself, or you can do it for them. Jab the pen through their clothes or on the bare skin. Hold in place for 10 seconds then rub for 10 seconds and throw the pen away in a sharps container. The person will feel relief, but still make sure you called 911. Click for Photo Reference
What it is: Diabetes mellitus is a chronic and currently incurable condition in which the body is unable to regulate the glucose (sugar) levels in the blood. It occurs when the pancreas doesn't make enough or any of the hormone insulin, or when the insulin produced doesn't work effectively. In diabetes, this causes the level of glucose in the blood to be too high. It is managed by a healthy lifestyle and balanced diet, sometimes requiring tablets or insulin.
1. Hyperglycemia (high blood sugar)
2. Hypoglycemia (low blood sugar)
1. A history of diabetes – casualty may recognize onset of ‘hypo’ attack
2. Hunger (A missed or late meal can cause the onset of a ‘hypo’ attack for a diabetic.)
3. Shallow breathing
4. Weakness, faintness or hunger
5. Palpitations and muscle tremors
6. Strange behavior – may seem confused or belligerent
7. Sweating and cold clammy skin
8. Pulse may be rapid and strong
9. Deteriorating level of response
Low blood sugar, known as hypoglycemia, can occur in diabetics when they use too much insulin, exercise too hard or too long, or have not eaten enough food. Hypoglycemia can develop quickly in people with diabetes.
Symptoms of low blood sugar typically appear when the sugar level falls below 70. Watch for:
1. Weakness
2. Shaking
3. Sweating
4. Headache
5. Nervousness
6. Hunger
If these symptoms occur and you have a blood sugar test kit available, do a blood sugar check. If the level is low, the person with diabetes should eat something with sugar: fruit juice, several teaspoons of sugar, a cup of skim milk, or regular soda. If you don't have a test kit handy, sugar should be eaten anyway — it can't hurt. Symptoms should subside within 15 minutes. If the symptoms don't subside, more sugar should be eaten and the sugar level tested again.
AFTER the symptoms subside, more substantial food can be eaten. Eat simple sugar FIRST to get the situation under control. Even if you or the person is hungry, "real" food should not be eaten until the sugar level comes up — real food won't produce enough sugar and takes too long to digest. If casualty improves, give him/her more to eat and drink. Watch for complications:
1. If condition does not improve look for other possible causes.
2. If consciousness is impaired, do not give anything to eat or drink
3. If unconscious, carry out ABCD’s, remembering to call for an ambulance.
Some heart attacks are sudden and intense — the "movie heart attack," where no one doubts what's happening. But most heart attacks start slowly, with mild pain or discomfort. Often people affected aren't sure what's wrong and wait too long before getting help. Here are signs that can mean a heart attack is happening:
1. Chest discomfort. Most heart attacks involve discomfort in the center of the chest that lasts more than a few minutes, or that goes away and comes back. It can feel like uncomfortable pressure, squeezing, fullness or pain.
2. Discomfort in other areas of the upper body. Symptoms can include pain or discomfort in one or both arms, the back, neck, jaw or stomach.
3. Shortness of breath. May occur with or without chest discomfort.
These may include breaking out in a cold sweat, nausea or lightheadedness. As with men, women's most common heart attack symptom is chest pain or discomfort. But women are somewhat more likely than men to experience some of the other common symptoms, particularly shortness of breath, nausea/vomiting, and back or jaw pain. If you or someone you're with has chest discomfort, especially with one or more of the other signs, don't wait longer than a few minutes (no more than 5) before calling for help. Call 911... Get to a hospital right away. Calling 911 is almost always the fastest way to get lifesaving treatment. Emergency medical services staff can begin treatment when they arrive — up to an hour sooner than if someone gets to the hospital by car. The staff are also trained to revive someone whose heart has stopped. Patients with chest pain who arrive by ambulance usually receive faster treatment at the hospital, too.
The American Stroke Association says these are the warning signs of stroke:
1. Sudden numbness or weakness of the face, arm or leg, especially on one side of the body.
2. Sudden confusion, trouble speaking or understanding.
3. Sudden trouble seeing in one or both eyes.
4. Sudden trouble walking, dizziness, loss of balance or coordination.
5. Sudden, severe headache with no known cause. If you or someone with you has one or more of these signs, don't delay! Immediately call 9-1-1 or the emergency medical services (EMS) number so an ambulance (ideally with advanced life support) can be sent for you. Also, check the time so you'll know when the first symptoms appeared. It's very important to take immediate action. If given within three hours of the start of symptoms, a clot-busting drug can reduce long-term disability for the most common type of stroke.
Cardiac arrest strikes immediately and without warning. Here are the signs:
1. Sudden loss of responsiveness (no response to tapping on shoulders).
2. No normal breathing (the victim does not take a normal breath when you tilt the head up and check for at least five seconds). If these signs of cardiac arrest are present, tell someone to call 911 and get an AED (if one is available) and you begin CPR immediately. If you are alone with an adult who has these signs of cardiac arrest, call 911 and get an AED (if one is available) before you begin CPR. Use an AED as soon as it arrives.
Heat stroke is the most dangerous of the heat-related illnesses. If not treated immediately, it can be fatal. The exact cause of heat stroke isn't clear, and unlike heat exhaustion, it strikes suddenly and with little warning. When the body cooling systems fails, the core temperature rises quickly. Signs of heat stroke include a core body temperature above 40.5°C / 104°F, hot, dry skin, lack of sweating, and a very fast pulse, and mental status changes.
Heat exhaustion may be difficult to differentiate from heat stroke, but it typically occurs when one is exposed to heat for a prolonged period of time. The body may become overwhelmed by heat when its mechanism (sweating) for keeping cool breaks down. Symptoms of heat exhaustion include nausea, dizziness, weakness, headache, pale and moist skin, weak pulse, and disorientation. The key difference between heat stroke and heat exhaustion is that there are no mental status changes (other than mild confusion) in those suffering from heat exhaustion. Stopping activity, and cooling the body are the key treatments for heat exhaustion (Have victim lie down, apply cold compresses, use a fan to lower temperature, elevate feet, have victim drink fluids). Click for Photo Reference
1. Always acclimatize for up to a week when exercising in hot weather conditions. This allows your body to gradually adapt to the heat.
2. Hydrate well before thirst kicks in. Once you are thirsty you are already dehydrated.
3. Do not exercise vigorously during the hottest time of day. Try to train closer to sunrise or sunset.
4. Wear light, loose clothing, such as cotton, so sweat can evaporate. Better yet, invest in some clothes that wick, like Cool-Max.
Occurs when skin is damaged from extreme cold. You want to re-warm the hands by a fire or with warm water.
Do not use hot water or rub them together (do not massage it). This will damage the skin more. If it becomes worse where the ends of the fingers or toes are becoming black, you need to go to the hospital or call 911 right away. Click for Photo Reference
Dial 911 immediately and immobilize the broken bone with a splint. A functional splint can be made of almost any material (wood, plastic, etc.) as long as it is rigid and is longer than the broken bone. To apply the splint simply lay it along the broken bone and wrap it against the limb with gauze or a length of cloth, starting at a point farthest from the body. Do not wrap it too tight as this may cut off blood flow. (snug, but not too tight!)
If the break is in the forearm, loosely wrap a magazine or a thick newspaper around the break and use a sling fashioned from gauze, ace bandage or a strip of cloth to keep the elbow immobilized. Click for Photo Reference
A break in the lower part of the leg requires two splints, one on each side of the leg (or at least the chin). If suitable material is not available, you can use the victim's healthy leg as a makeshift splint. If you have to splint it, remember to splint it ABOVE AND BELOW the injury.
As much as possible, keep the victim from moving and until an ambulance arrives, remember ICE:
"I" is for ice — if possible apply an ice pack or ice cubes to the injured area. This will keep down the swelling and reduce pain.
"C" is for compression — if the wound is bleeding, apply direct pressure with a clean cloth to reduce blood flow.
"E" is for elevation — try to keep the injured area as high above heart level as possible.
A burn victim will require different type of care depending on the type and extent of his injury. Burns vary greatly from a common, fairly harmless sunburn to a potentially life-threatening 3rd degree burn caused by open flames or electrocution. Here's how to distinguish the three different types of burn injuries and how to care for each:
1st degree burns are usually accompanied by redness and some swelling of the skin. Treat a minor burn by first cooling the affected area. If possible, keep the injury under cool running water for at least 10 minutes. If running water is not available place the burn in a container of cold water such as a bucket, tub or even a deep dish. Using a cool, wet compress made of clean cloth will also work if nothing else is available. Keeping the burn cool will reduce pain and minimize the swelling. If the injury is on the part of a body where jewelry or snug clothing is present, carefully remove them before it begins to swell. Apply a moisturizing lotion or Aloe Vera extract and dress the burnt area with loosely wrapped sterile gauze.
2nd degree burns will result in deeper, more intense redness of the skin as well as swelling and blistering . This type of burn should be treated just as a 1st degree burn but because the damage to the skin is more extensive, extra care should be taken to avoid infection and excessive scarring. Replace the dressing daily and keep the wound clean. If a blister breaks use mild soap and warm water to rinse the area. Apply antibiotic cream such as Neosporin to prevent infection before redressing in sterile gauze.
3rd degree burns may appear and feel deceptively harmless as the victim may not feel much pain due to complete destruction of all layers of skin and tissue as well as nerve endings. The damaged area may appear charred or ash-color and will instantly start to blister or "peel". If the victim's clothing is on fire, douse him with non-flammable liquid. Dial 911. Do not remove burnt clothing from the victim as this will expose open wounds to the elements and potential infection. If possible, cover the victim's injuries with wet sterile cloth to reduce the pain and swelling. If you notice that the victim is going into shock and loses consciousness, you will need to perform CPR. Click for Photo Reference
Is usually caused by a piece of foreign matter such as food becoming lodged in a person's windpipe. Because a choking victim is fully aware that he cannot breathe normally, a sense of panic may overcome them, making assessing the situation and rescue efforts difficult. It is important to try and keep the victim calm in order to determine whether your assistance is truly necessary or if the victim's own coughing reflex is sufficient.
Start by asking the person if he is choking. This simple step can be deceptively effective — the victim may be coughing violently or even gasping for air, but if he is able to answer then he is probably not choking. A choking victim will not be able to speak since oxygen cannot reach his lungs. But if after asking the person if he's choking all he can do is gesture or point to his throat and you notice his face starting to turn blue, then he is most likely choking and you will need to perform the Heimlich Maneuver immediately. Click for Photo Reference
The first and most important step when treating minor cuts and scrapes is to thoroughly clean the wound with mild anti-bacterial soap and water. You can use sterilized tweezers to remove any debris that remains embedded in the wound after rinsing. This will reduce the risk of an infection and possible complications. If the debris is abundant or can't be removed for some other reason, a trip to the emergency room will be necessary. Water may induce bleeding by thinning the blood. If while rinsing the wound you notice increased blood flow, use gauze or a clean cloth to apply gentle, continuous pressure until the blood clots.
Although hydrogen peroxide is commonly used as a disinfectant for minor cuts and scrapes, it is actually not very effective and may even delay the healing process by irritating a person's living cells. You can use hydrogen peroxide but apply it around the open wound, not directly to it. An antibiotic ointment such as Neosporin is a better alternative — it will keep the wound from getting infected and speed up the healing process. Dress the wound with a bandage or sterile gauze to keep dirt and bacteria out. Change the dressing frequently and rinse the wound as often as necessary to keep it free of dirt. Continue to monitor the wound for several days. If the injured area turns red or puffy, or if excessive pain persists, then it may have become infected and will require a physician's attention. Do not simply dismiss cuts as minor injuries as some may be quite serious if not tended to by a professional. If the wound is very deep or the bleeding is profuse, it may require stitches in order to heal properly.
Click for Photo Reference
A human nose is rich with small fragile blood vessels which are susceptible to damage. A nosebleed may be caused by a fall, a strike to the nose, or even from breathing excessively dry air. If the nosebleed is not a symptom of a more serious injury, it is rarely dangerous and can usually be stopped by applying continuous pressure.
1. Do NOT tilt the victim's head backward.
2. Pinch the nostrils shut and press the tip of the nose against the bones of the face.
3. Maintain pressure for 5 to 10 minutes.
4. Once the bleeding has stopped, the victim should avoid blowing his nose or otherwise straining himself for at least an hour.
Click for Photo Reference
Always wear gloves and dispose of everything in a bio hazard bag (red).
To stop bleeding, first use gauze. If it keeps bleeding, add more gauze on top and raise the injured area if it is not broken.
Remember these steps:
1. Apply pressure. Next step is to used rolled bandage on top of the sterile gauze.
2. If this does not work, add more gauze or elevate the arm or leg.
3. If this still does not work, use the brachial pressure point (between bicep and tricep near the armpit) or femoral artery (inside of groin in the leg).
Place the orange tip against the middle of the outer thigh (upper leg) at a right angle (perpendicular) to the thigh. Swing and push the auto-injector firmly until it “clicks.” The click signals that the injection has started. Hold firmly in place for 3 seconds (count slowly 1, 2,3)
This medication is used in emergencies to treat very serious allergic reactions to insect stings/bites, foods, drugs, or other substances. Epinephrine works quickly to improve breathing, stimulate the heart, raise a dropping blood pressure, reverse hives, and reduce swelling of the face, lips, and throat.
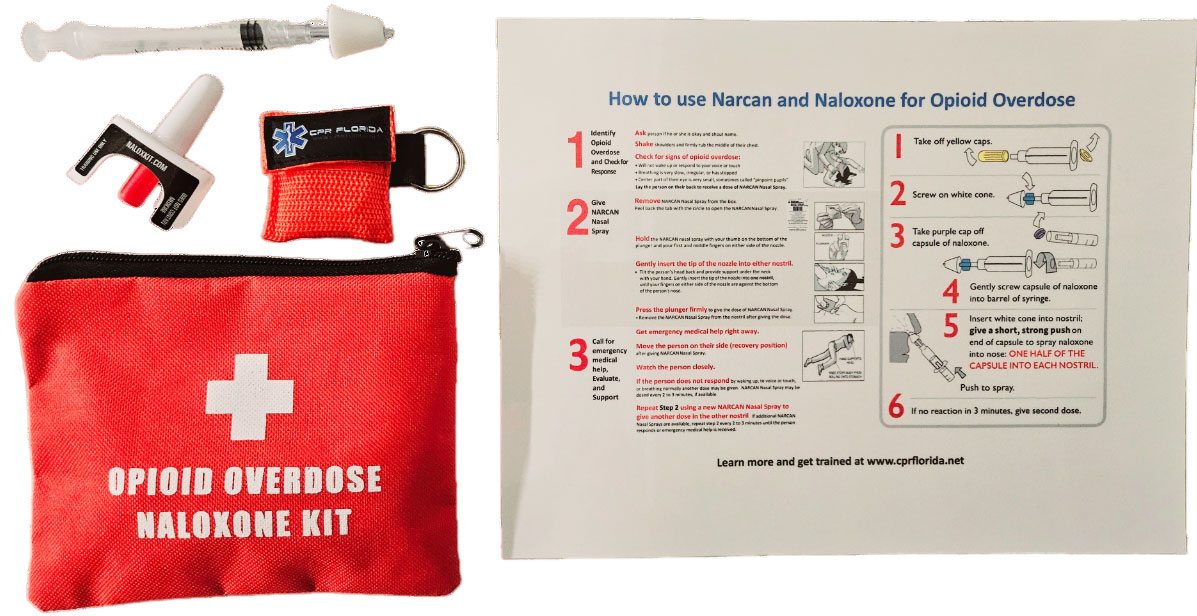
First, what is this drug? Naloxone, for example Narcan®, is a medicine that can help people who are overdosing on an opioid. Opioids include prescription medications, heroin, and fentanyl. Sometimes other drugs, including cocaine and methamphetamine, are mixed, or laced with fentanyl. 2.
Naloxone is a medicine that rapidly reverses an opioid overdose. It is an opioid antagonist. This means that it attaches to opioid receptors and reverses and blocks the effects of other opioids. Naloxone can quickly restore normal breathing to a person if their breathing has slowed or stopped because of an opioid overdose. But, naloxone has no effect on someone who does not have opioids in their system, and it is not a treatment for opioid use disorder. Examples of opioids include heroin, fentanyl, oxycodone (OxyContin®), hydrocodone (Vicodin®), codeine, and morphine.
ONLINE CLASS: We also now have a totally online & fully accredited options!
Here is more info about how to sign up for a bloodborne pathogens hands on class or online class
ONLINE CLASS: We also have a totally online & fully accredited option! Click on the icon for the online bloodborne pathogens courses for all professions including tattoo artists body art piercers www.bloodbornepathogensonline.net
Here are several diseases that are caused by Bloodborne pathogens (BBP's). While many BBP's are fairly exotic and you may never encounter them, a few BBP's are fairly common and present a risk to you if you come in direct contact with potentially infectious materials such as human blood and certain body fluids. Occupational Safety and Health Administration (OSHA) has recognized that health care workers and others, who may in contact with human blood or blood associated materials (Other Potentially Infectious Materials or OPIM for short) has recognized this occupational hazard and created the " Bloodborne Pathogen Standard ".
This standard has served as the basis for implementing policies and practices to minimize your risk of exposure to BBP's, specifically to Hepatitis B virus (HBV), Hepatitis C virus and Human Immunodeficiency Virus (HIV). These policies and practices, if followed, are an effective means to reducing your risk of exposure to other pathogens as well.
Take off first glove starting at the top near the wrist. Make the glove inside out and place it inside the other gloved hand. Remove the other glove by slipping your bare fingers inside the glove at the top of the wrist and pull it off so that it is inside out. The gloves should be inside of each other. Any lightly soiled bandages or band aids should be inside the gloves. Put in biohazard bag. Blood and Other Potentially Infectious Materials (OPIMs) HIV and HBV may be found not only in human blood, but also in other potentially infectious materials including the following body fluids:
1. Blood products (such as plasma or serum)
2. Semen
3. Vaginal secretions
4. Cerebrospinal fluid
5. Pleural fluid (or lung fluid)
6. Synovial fluid (or fluid from your joints)
7. Amniotic fluid (or uterine fluid)
8. Peritoneal fluid (or fluid that fills your body cavity)
9. Saliva in dental settings
10. Any body fluid that is visibly contaminated with blood
11. Any body fluid that you can't tell what it is
Other items found in the clinical or laboratory setting are also considered to be other potentially infectious materials (OPIM) and they include:
1. Any unfixed tissue or organ, other than intact skin, from a living or dead person
2. Cell or tissue cultures that may contain Bloodborne pathogens as outlined in LBNL's Exposure Control Plan
3. Organ cultures and culture medium or other solutions that may contain HIV or HBV blood from experimental animals infected with HIV,
4. HBV or other BBPs.
It is a required practice to use Universal Precautions when handling these body fluids and materials. The following body fluids are not expected to be infectious sources of Bloodborne pathogens unless they are visibly contaminated with blood:
1. Urine
2. Feces
3. Vomit
4. Tears
5. Sweat
6. Sputum
7. Nasal secretions
Although these body fluids do not currently require universal precautions, good personal hygiene practices are highly recommended when handling these materials.
Bloodborne pathogens can be transmitted when infectious blood or OPIM is introduced into the bloodstream of a person. Transmission of Bloodborne pathogens in the workplace can occur through the following routes of transmission:
1. Parenteral exposure - this means that the infected blood or OPIM is introduced directly into your body through a break in the skin. Examples include: a needle-stick injury or a cut with a piece of contaminated glass.
2. Mucous membrane exposure — this means that the infected blood or OPIM enters your body through contact with a mucous membrane found in your eye, nose or mouth.
Bloodborne pathogens may also be transmitted through:
1. Sexual contact
2. Infected women may expose their newborn children to BBP's through amniotic fluid, through blood during the birthing process, and (less likely) through breast milk.
HIV is the virus that gradually weakens the immune system of the infected person, leaving that person unable to fight off other infections. This leads to acquired immunodeficiency syndrome (AIDS) and will ultimately cause death. HIV-infected persons may have no symptoms or may experience symptoms such as swollen lymph nodes, fatigue, weight loss, diarrhea, persistent dry cough and fever.
According to CDC statistics, HIV-related illness was the leading cause of death among young adults between the ages of 25 and 44 years old in 1995. It is still the second leading cause of death for this age group today.
HBV Hepatitis B virus (HBV) is a virus that causes an infection of the liver potentially leading to liver disease, liver cancer and possibly death.
Symptoms of HBV infection may range from no symptoms, to brief flu-like symptoms, to jaundice and serious illness. If symptoms do occur, they may not be evident until 2 to 6 months after the person is infected. However, studies have shown that an infected person can be infectious to others several weeks before the onset of symptoms.
CDC estimates that between 140,000 and 320,000 people become infected every year in the U.S. Approximately one-half of all people who become infected do not have any symptoms of infection. Approximately 10% of all people who become infected may become "carriers" of HBV. This means that they may suffer from infection at a later time (chronic infection). They can also be infectious to others for the rest of their lives while not necessarily demonstrating any symptoms of HBV infection themselves.
Individuals whose jobs involve handling blood and OPIM are at a much greater risk of becoming infected with HBV than HIV. Why you may ask? It is because there are many more HBV-infected people than HIV-infected people in the community. Thus the chance of exposure to HBV is greater. Also Hepatitis B virus is much more infectious than HIV. This difference in infection risk is best illustrated by the following statistics:
1. If you had a needle stick accident and were exposed to infected blood, your chance of acquiring an infection would be: 0.3% or 3 in 1000, HBV 30.0% or 300 in 1000. According to CDC, your risk for acquiring an HBV infection is 100 times greater than for HIV. When considering the risk of occupational exposure to HBV, keep in mind that a safe and effective vaccine is available to you.
A 3-shot vaccination series is available for hepatitis B virus. The vaccination is highly effective and safe. As an employee encountering blood and potentially infectious materials in the course of your job, you are entitled to the vaccination at no cost.
Hepatitis C virus (HCV), also formerly known as "non A-non B", is another pathogen that you need to be aware of if you have occupational exposure to human blood or other potentially infectious materials. Hepatitis C virus has been found in all parts of the world. The virus appears to be transmitted most efficiently through parenteral exposure to blood from an infected individual. Common examples of transmission events are: receiving a blood transfusion from an infected source or sharing intravenous drug needles with an infected individual.
Like HBV, symptoms of HCV can range from no symptoms or flu-like symptoms to jaundice and even death in rare instances. Also similar to HBV, HCV has a carrier state which can lead to chronic infection and liver disease. Unlike HBV, there is currently no vaccine for HCV available and immune globulin administered after exposure does not appear to be very effective in preventing HCV infection.
Although the risk of HCV transmission is still being defined, the risk of transmission by the following routes appears to be low:
1. Regular household contact situations
2. Sexual contact
3. Passing the infection from mother to unborn child
4. Cases of transmission of HCV to health care workers have occurred through accidental needle sticks, cuts with sharp instruments, and splashes to the eye with human source material.
1. How long does HIV or Hepatitis B or C last on surfaces or in the air?
HIV does not last long at all in the air or on surfaces. It must be contained in the blood to infect someone. Hepatitis A, Hepatitis B and Hepatitis C are all forms of viral hepatitis — an inflammation of the liver caused by a virus. However, there are a number of characteristics that differentiate these diseases. Hepatitis A — is spread by a fecal-oral route or by eating and drinking contaminated food or water. In younger patients the infection often goes unnoticed. Most patients recover fully after a short illness. As a result of their infection, they develop lifelong immunity. Hepatitis B — is transmitted through infected blood and body fluids. It can be passed, for example, from mother to child during delivery. It can also be transmitted sexually, and is therefore a sexually transmitted disease. Hepatitis B is often spread through injection drug use. The majority of adults infected with the Hepatitis B virus recover completely, and as a result of their infection, develop lifelong immunity to the virus. However, approximately 10% of adults and 90% of infants who become infected with Hepatitis B cannot get rid of the virus and are considered to have chronic Hepatitis B. These people become long-term carriers, and although they may be symptom free for many years, they may develop cirrhosis or liver cancer later in life.
2. Is there a cure for Hepatitis C?
Current treatment includes a combination of anti-viral drugs (interferon and ribavirin) and approximately 40% of people receiving this treatment are able to completely eliminate the Hepatitis C virus from their bodies. Success ranges from 20-80% and depends on many factors: the amount of scarring in the liver, the amount of virus in the body and the specific genotype of Hepatitis C. Most people with Hepatitis C can live a healthy life for many years. Only about 20% of Hepatitis C patients develop cirrhosis or liver cancer. The key to successful treatment and management of the disease is early diagnosis and treatment.
3. Is there a vaccine for Hepatitis C?
There is no vaccine for Hepatitis C at the present time. Once in the body, HCV can literally change its coat (or outer capsule) in a process called mutation. It is this outer coating that helps the body or vaccine identify a virus and attack it. Thus, developing a vaccine for Hepatitis C has become a moving target. You would need a different vaccine for each mutation of the virus. Researchers are currently tackling this challenge but a vaccine is not expected in the near future.
4. How long can HCV live outside the body and transmit infection?
Recent studies suggest that HCV may survive on environmental surfaces at room temperature at least 16 hours, but no longer than 4 days. What do you use to remove HCV from environmental surfaces? You should clean up any blood spills — including dried blood, which can still be infectious — using 1:10 dilution of one part household bleach to 10 parts of water for disinfecting the area. Use gloves when cleaning up any blood spills. Go here to view more info on Hepatitis: View more info here
View how to do CPR and spine board the patient is in a pool if you are a lifeguard or EMT.
View steps here
You must know adult, child and infant CPR. You must know advanced first aid. You must also know 2 person CPR, bag/valve mask, CPR one way valve mask, and AED. You must also know about advanced airways and intubation. Additional components are: oxygen administration, oral and nasal adjuncts and suction devices.
These curved pieces of rigid plastic are inserted into the mouth of a patient who has lost their gag-reflex (often because they are unconscious) to protect them from occluding their own airway as the muscles of the tongue and to relax.
These soft flexible rubber tubes are lubricated and inserted in through a patient's nostril with the same purpose as the OPAs above. They are designed to provide a protected airway through which the patient may breathe, naturally or with the help of emergency rescuers. The advantage to using an NPA is that a patient with an intact gag-reflex who will reject an OPA may still be provided with an airway.
If a patient develops fluid in their mouth or throat, it is often necessary to remove the fluid in order to prevent aspiration into the lungs. This is accomplished using a suction device. Most ambulances will carry an electric suction device, but for reasons of portability our organization uses a hand-pump device which accomplishes the same task.
Oxygen is most commonly given by nasal cannula, which is a plastic tubing that reaches to the nostrils. It is also given by a mask, which covers the mouth and nose. In both cases, the nasal cannula or mask are attached to plastic tubing which attaches to a source of oxygen: oxygen tanks of various sorts or oxygen concentrators. Oxygen is given at a certain speed or rate which is measured in liters per minute.
Oxygen should be delivered with properly sized equipment for the respective victims and appropriate flow rates for the delivery device.
Resuscitation mask: flow rate 6 -15 LPM, 35-55 percent oxygen concentration, breathing and non-breathing victims
Non-rebreather mask: flow rate 10-15 LPM, 90+ percent oxygen concentration, breathing victims only
BVM: flow rate 15 LPM or more, 90+ percent oxygen concentration, breathing and non-breathing victims
A nasal cannula is a plastic tube with two small prongs that are inserted into the victim?s nose. This device is used to administer oxygen to a breathing victim with minor breathing problems.
Oxygen is normally delivered through a nasal cannula at a low flow rate of 1 to 6 LPM.
Nasal cannulas also can be used if the victim does not want a mask on his or her face.
A resuscitation mask with an inlet valve may be used with emergency oxygen to give rescue breaths to breathing and nonbreathing victims.
The recommended flow rate when using a resuscitation mask is 6 to 15 LPM.
A non-rebreather mask is an effective method for delivering high concentrations of oxygen to a breathing victim.
Non-rebreather masks consist of a face mask with an attached oxygen reservoir bag and a one-way valve, which prevents the victim?s exhaled air from mixing with the oxygen in the reservoir bag. Flutter valves on the side of the mask allow exhaled air to escape freely. As the victim breathes, he or she inhales oxygen from the bag.
Because young children and infants may be frightened by a mask being placed on their faces, consider a blow-by technique. The rescuer, parent or guardian should hold a non-rebreather mask approximately 2 inches from the child?s or infant?s face. This will allow the oxygen to pass over the face and be inhaled.
The reservoir bag should be sufficiently inflated (about two-thirds full) by covering the one-way valve with your thumb before placing it on the victim?s face. If it begins to deflate when the victim inhales, increase the flow rate of the oxygen to refill the reservoir bag.
The flow rate when using this device is 10 to 15 LPM.
A non-rebreather mask can deliver an oxygen concentration of 90 percent or more.
A BVM can deliver up to 100 percent oxygen to a breathing or non-breathing victim when attached to emergency oxygen.
Squeezing the bag as the victim inhales helps deliver more oxygen. BVM flow rates should be set at 15 LPM or more.
It is very important to follow the physician's orders about how much oxygen to given per minute. Click for Photo Reference
Like the Pocket Mask, the BVM includes a face mask with a one-way valve. The key difference is that the air for respirations comes from the bag and reservoir, which can be attached to an oxygen tank for high concentration oxygen, rather than from the rescuers own lungs. (it also does not have to have oxygen...either way, it is better for the patient.) This method of delivery is often much more effective, contains more oxygen and is more beneficial especially if there are multiple rescuers on scene. Click for Photo Reference
ACLS VIDEOSRemember, we will travel to your site anywhere in Florida. We are located in South Florida, in West Palm Beach and teach American Heart Association (AHA), American Safety and Health Institute (ASHI) and American Red Cross certified CPR courses. We also teach CPR and first aid to child care and day care centers in South Forida and West Palm Beach Florida. We have locations in West Palm Beach, Miami, Fort Lauderdale, Jupiter, Boynton Beach, Wellington, Stuart, Orlando, Fort Pierce and Sebastian areas. Click Here to Sign Up Now!
The office cpr scene: https://www.youtube.com/watch?v=ssIY8NYwvh4
Jumunji cpr scene: https://www.youtube.com/watch?v=5YgMl4JQxKw
duplex movie choking and cpr http://www.youtube.com/watch?v=aB1imaHkwlU
aha hands only cpr http://www.youtube.com/watch?v=n5hP4DIBCEE&feature=related
Dumb and Dumber cpr http://www.youtube.com/watch?feature=endscreen&NR=1&v=m-HmvPr7mG0
mr bean cpr http://www.youtube.com/watch?v=FnAOmxnQJsM
bondi cpr - austrailian live cpr aed www.youtube.com/watch?v=ICODRFoWZkw
Real live cpr - man collapses at desk at work and co workers help save him
Live cpr and aed use by teachers. They save a 7th grader in the hallway!
Pediatric video with bls and aed use
cpr bls first aid coupon promo code
pet cpr
Cops Save Life on side of road
girl (17 years old) has SCA and dies on the volleyball court all caught on video
BLS and ACLS overall review and help to pass the tests: https://www.youtube.com/watch?v=1MnXq29TbcU
Yes, we can travel to you or we have offices in Pompano Beach, Miami, Coral Springs, Tallahassee, West Palm Beach, Fort Lauderdale and Tallahassee where you can learn cpr and bls near me https://cprflorida.net/cprblsclassesnearme


